Rheumatoid arthritis and its effects on oral health
Published: 01/02/2014
Rheumatoid arthritis is an autoimmune condition associated with periodontal disease and dry mouth. In addition, patients can find oral health care difficult. Dental care professionals need to be able to advise patients about oral health and products that can assist them
Rheumatoid arthritis (RA) is an autoimmune disease of the arthritis family. It is a condition where a patient's own immune system attacks the body, in this instance the joints. The resulting inflammation of the joints can be painful and debilitating, leading to weakness and consequently a loss of function. If the hands are affected, it can have an impact on oral health.
There is a link between people with RA and periodontal disease (Mercado et al, 2000), which means that members of the dental team need to manage patients reporting this disease in their medical history carefully.
What is rheumatoid arthritis?
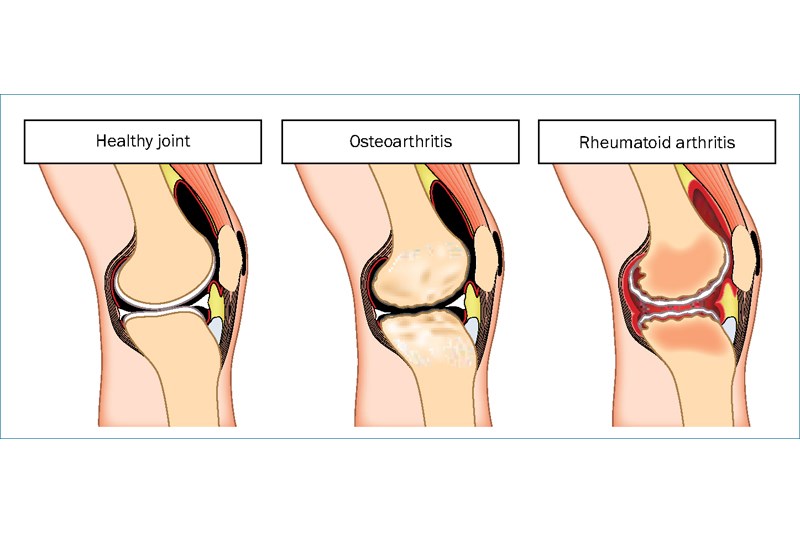
The term arthritis is defined as a serious condition in which a person's joints, the places where two bones are connected, become painful, swollen and stiff (Cambridge Dictionaries Online, 2013) (Figure 1).
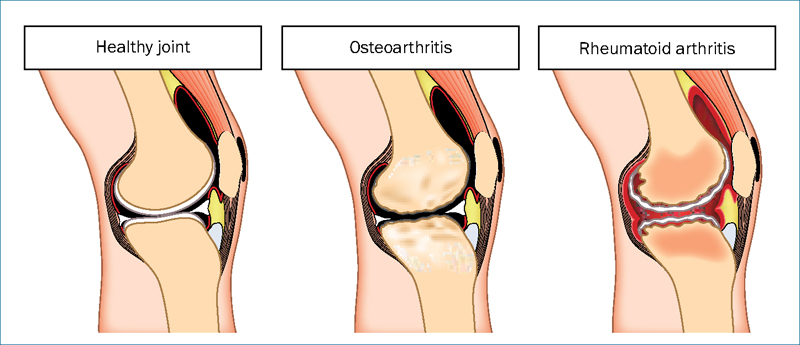
Figure 1.Healthy joint; osteoarthritis; RA
There are many types of joint conditions that go under the term of arthritis, the most common being osteoarthritis and rheumatoid arthritis. They are often confused, but are different.
Osteoarthritis is characterised as wear and tear of the joints, and is believed to affect more than 8.5 million people in the UK (NHS Choices, 2012a); the damage often increases with age, necessitating replacement joints, commonly to the hip and knee.
Rheumatoid arthritis affects approximately 387 000 people in the UK (Arthritis Research Campaign, 2000). Its onset typically occurs around midlife, but can affect people at any point in life. Women are three times more likely to be affected than men, and it is estimated that there are approximately 20 000 new cases each year (Arthritis Research UK, 1999).
Rheumatoid arthritis is different from osteoarthritis in that it is an inflammatory form of the condition where the tissues surrounding the joint become inflamed. This is an autoimmune response, which can be described as ‘the body fighting the body’. The immune system perceives that the body is under attack, and launches an inflammatory response. In reality, the immune system has misinterpreted the threat and is attacking the body's own cells and tissues (Research Council of Norway, 2011).
This inflammatory response can be destructive to the joint over time, causing pain, swelling and ultimately deformity (Figure 2). It causes chronic and acute inflammation, typically in the extremities—hands, wrists, knees and feet.
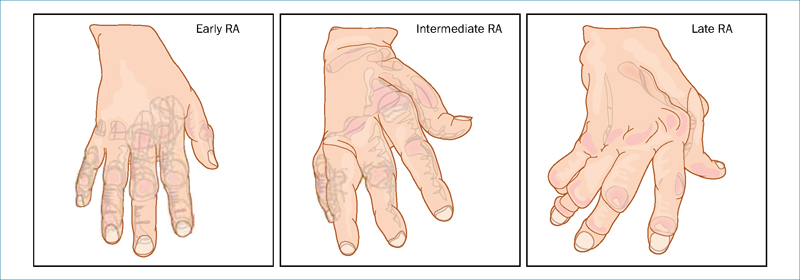
Figure 2.Stages of rheumatoid arthritis
The cause is as yet not fully understood, but it is thought that genetics may be involved. The severity of the disease can vary considerably from one patient to another.
Signs and symptoms
The condition is characterised by acute or chronic swelling and inflammation of the joints, leaving them painful, stiff and often hot and red in an acute phase, which is called a flare-up. During the acute phase, patients can feel very fatigued and generally unwell. Flare-ups may occur in different sets of joints, and move around the body.
Diagnosis
Diagnosis is undertaken by a GP, initially via a physical examination of the joints and a series of blood tests, typically erythrocyte sedimentation rate (ESR) and/or C-reactive protein (CRP) tests. These indicate the levels of inflammation in the body.
A more specific but not definitive test is to see whether rheumatoid factor is present in the patient's blood. Rheumatoid factor is an antibody, detectable in 80% of adults with RA (MedicineNet.com, 2013). High levels can indicate a more aggressive form of the disease. However, as this antibody is found in one in 20 people who do not have RA (NHS Choices, 2012b), it is not necessarily a confirmation of the disease.
Radiographs might also be taken to see if there has been any damage to the joints. The GP may refer the patient to a consultant rheumatologist for more specialist management of the condition.
Management
Rheumatoid arthritis is commonly treated with drug therapy.
The early stages are controlled with painkillers and non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, or COX-2 inhibitor NSAIDS, which carry a lower risk of serious stomach problems (NHS Choices, 2012c). These reduce pain and swelling in the affected joints.
As the condition progresses, disease-modifying anti-rheumatic drugs (DMARDs) may be used, either singly or in combination. DMARDs work by suppressing the immune system and therefore the body's reaction, easing swelling, stiffness and pain in the joints. These drugs can slow down the progression of the disease and therefore the rate of damage to the joints. They are for long-term use, and may take several months to work fully. However, because of potential side effects, patients taking them needs to be closely monitored with regular blood tests.
Corticosteroids are also commonly used to suppress inflammation when several joints are involved, and can be given orally or by injection into the muscle.
In recent years, a new type of drug regime has been developed called biological therapy. These treatments work by preventing certain chemicals in the blood from activating the immune system and attacking the lining of the joint (NHS Choices, 2012c).
Table 1.
Common drugs used to treat rheumatoid arthritis
| NSAIDs | Corticosteroids | DMARDs | Biologies |
|---|---|---|---|
| lbuprofen | Prednisolone | Sulfasalazine | Rituximab |
| Naproxen | Methotrexate | Tocilizumab | |
| Diclofenac | Leflunomide | Adalimumab | |
| COX-2 inhibitors | Hydroxychloroquine | Etanercept | |
| Celecoxib | Infliximab | ||
| Etoricoxib |
Physiotherapy and exercise can be beneficial to preserve movement in the joints.
Occupational therapy can help patients to adapt to everyday life in a way that will help protect the joints. Affected joints can become weakened and there are aids to assist with tasks such as removing tight lids on food containers, lifting heavy kettles or turning on taps.
In some cases, surgery is performed to remove the inflamed joint tissue or replace damaged joints.
Impact on oral health
The difficulties that limited and painful joints cause can significantly affect everyday oral home care. This can result in poor oral hygiene and therefore affect oral health, with an increased risk of caries and periodontal disease.
Secondary Sjögren's syndrome (which causes dry eyes and mouth) is often associated with people who have autoimmune conditions such as RA (WebMD, 2012). The reduced saliva flow is linked to an increased risk of caries, as its cleansing mechanisms and antibacterial effect and reduced.
Link between RA and periodontal disease
It is becoming more apparent that there are links between periodontal health and systemic health. A number of studies have shown a link between rheumatoid arthritis and periodontitis (Rajkarnikar et al, 2013).
An Australian study in 2 000 looked at 1 412 patients who were attending the University of Queensland School of Dentistry (Mercado et al, 2000). They were assessed for evidence of periodontal disease and RA. Some were attending for periodontal treatment, others for routine dentistry.
‘Growing evidence on links between rheumatoid arthritis and periodontal disease means careful monitoring is necessary’
The prevalence of RA was significantly higher in the group who were referred for periodontal treatment than in the group who were attending for regular dentistry. Of those who were referred for periodontal treatment who had RA, 62.5% presented with an advanced form of periodontal disease.
It is thought that this link derives from the impaired inflammatory response of RA patients and the inflammatory nature of periodontitis. The researchers concluded: ‘There was good evidence to suggest that individuals with moderate to severe periodontal disease are at higher risk of suffering from rheumatoid arthritis and vice versa’ (Mercado et al, 2000).
How the dental team can assist patients
Stiffness is generally worse in the morning so afternoon appointment times might be considered. RA can make joints in the knees and neck painful so care in seating the patient in the dental chair will be appreciated. A cushion under the knee area or a memory foam neck support would make a long appointment time more comfortable.
Good oral home care is a fundamental part of managing dental health. This can be difficult for people with stiff hands. Pipe lagging foam, available from DIY stores, is a cheap and effective way of increasing the size of a manual toothbrush handle to provide a more comfortable grip (Figure 3). It can be taped round the handle, is waterproof and can be cleaned. Electric toothbrushes can be helpful as their handles tend to be wider and therefore easier to hold; the oscillating or sonic action reduces stress on the hands, increasing plaque removal.

Figure 3.Toothbrush handle customised with foam pipe lagging for comfort
Flossing can be extremely difficult for RA patients, as a good degree of dexterity is needed. Patients may find a floss pick, a pre-threaded flossing aid, more manageable than standard floss. They may also find air flossers or water flossers beneficial. The ease of use and the size of the handles of these products make them effective for patients with compromised hand movement.
There are specific mouthwashes, toothpastes and gels that can assist with dry mouth symptoms. For caries, fluoride toothpastes and mouthwashes are recommended. Antibacterial mouthwashes would be indicated for periodontal flare-ups.
sec-type="conclusions">Conclusion
Specific issues need to be considered when managing patients who have rheumatoid arthritis.
The growing evidence base on links between RA and periodontal disease means careful monitoring of this gingival condition will be necessary, as well as informing patients of their increased risk of potential periodontal problems. Regular reviews of the patient's home care routine, particularly in relation to their ability to manage oral care aids physically, can be beneficial.
The use of products to counter dry mouth and those with extra fluoride to help prevent caries can be used in a preventive regimen.
Advances in drug therapy mean that long-term suppression of the autoimmune response, and therefore reduced joint damage, pain and swelling, is becoming a realistic outcome for patients with this condition.
position="float" orientation="portrait">Key points
? Rheumatoid arthritis (RA) is an autoimmune disease of the arthritis family.
? It is characterised by pain, swelling and stiffness of joints.
? RA commonly affects hands, wrists, knees and feet.
? If the hands are affected, RA can make oral care difficult.
? Studies have shown a link between RA and periodontitis.
? Dry mouth can be associated with patients with RA.
Author: MA Healthcare
Please sign in or subscribe to continue reading.
The following article is restricted for Dental Nursing subscribers only. Please sign in to access the full article.
If you have any queries or require more information, Dental Nursing’s friendly customer services team is on hand to help. Call 01722 716997 or email subscriptions@markallengroup.com.
Subscribe to Dental Nursing below and get access to this article. Subscribing will enable you to:
- Update your knowledge in important areas of practice.
- Keep fully up-to-date with the latest developments taking place in clinical practice as they affect you.
- Access restricted content and our CPD platform.







.jpg?width=150&height=100&scale=canvas)